


Risk assessment for health plan’s member letters and notifications
Client background
A large, multi-state health plan covering more than three million lives.
The business challenge
The client set out to understand the various risks associated with the member letters and notifications distributed throughout the year. A key driver of the need for an assessment was the client’s decentralized environment, which included various systems, templates, roles and responsibilities for member letter development, compliance and standards review, and distribution. An additional driver was the client’s expansion into the Medicare Advantage and Medicaid lines of business. Baker Tilly was engaged to create a consolidated view and to perform an assessment of the associated processes in defined scoped areas of member letters.
The Baker Tilly approach
Baker Tilly’s overall approach was to support the client in understanding the associated risk related to the letters being sent to the members of their various health plans. Based on Baker Tilly’s understanding of the key objectives for the client and industry experience, Baker Tilly planned an approach that divided the work into five phases.
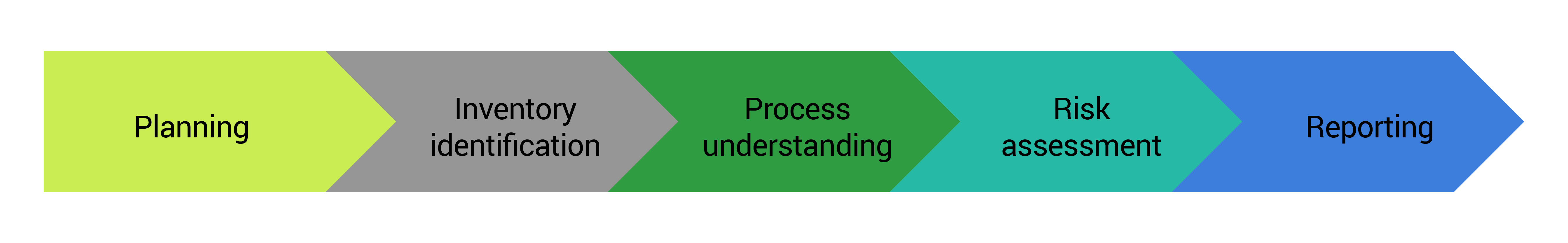
Planning:
Engaged with business department and functional leaders to understand organizational structure and refine approach for assessment.
Inventory identification:
Conducted stakeholder meetings and uncover over 3,000 letter templates being sent to members by way of 15 unique systems/processes.
Process understanding:
Created process maps for each of the identified processes and detail points of emphasis.
Risk assessment:
Both a qualitative and quantitative risk assessment was conducted on the inventory of member letters to provide risk scores in order to identify which letters had the highest risks based on factors such as:
- Process risks
- Regulatory risks
- Reputational repercussions
- Content accuracy
Reporting:
Risk assessment scores and process maps were used to compose actionable assessments for the impacted teams and collaborate with management to create action plans to address identified issues.
Business impact
Baker Tilly’s approach enabled the client to gain a bigger picture understanding of the letters being sent to their members and the supporting processes:
Centralized inventory:
Baker Tilly was able to take member letters from 15 different sources and create a singular source for the business to reference when reviewing and auditing their letter templates.
Enable scalable growth:
The client’s expansion into Medicare Advantage and Medicaid was driven through both internal expansion and external acquisition of other regional health plans. By expanding through different avenues, the client had several processes that served the same purpose. This assessment allowed the client to understand their duplicative processes and begin to create a plan for consolidation.
Process maps:
Prior to the engagement, most processes evaluated did not have formal policy and procedure documentation. The process maps created have served as primary inputs to the creation of these documents across the different business areas.
